The Editor,
I am writing to express my concerns regarding the recent calls to re-open səmiq̓ʷəʔelə/Riverview Hospital, which have emerged following a tragic and seemingly random murder and assault that occurred recently in Vancouver.
While such incidents understandably provoke strong reactions and calls for action, the notion of re-instituting səmiq̓ʷəʔelə/Riverview Hospital as a viable solution is fundamentally flawed and reflects a misunderstanding of contemporary mental health care, and the complexity of interacting social factors like social isolation, poverty, homelessness and decades of defunding social services, education and health care.
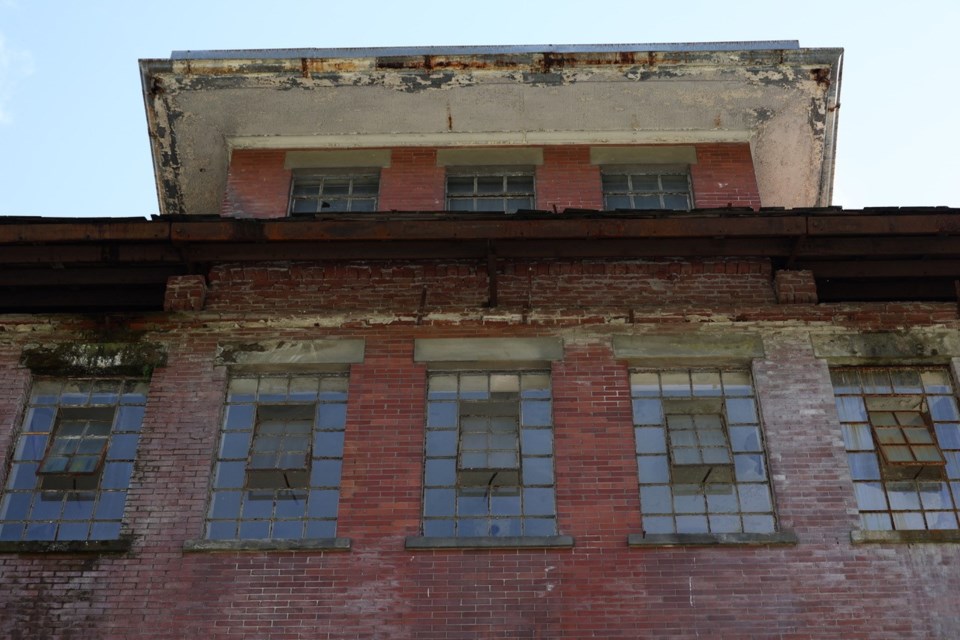
First and foremost, there is a mistaken belief that no effective mental health programs currently operate on the grounds that once housed səmiq̓ʷəʔelə/Riverview Hospital. In reality, inpatient rehabilitation-focused mental health programs have been operational on the old səmiq̓ʷəʔelə/Riverview Hospital grounds since the early 2010s. These programs are part of a modern, comprehensive approach to mental health care that includes a range of community-based services. Romanticizing the idea of "re-institutionalization" overlooks the fact that such a model requires significant financial investment and a highly trained mental health workforce. The current infrastructure already supports a continuum of care that could be scaled to meet the needs of individuals, integrating them into the community rather than isolating them in institutional settings.
Second, the idea that lifetime institutionalization is a viable solution for individuals with persistent mental health issues is deeply problematic. Such an approach overlooks the advancements in mental health treatment and the importance of integrating individuals into the community. Modern mental health care emphasizes recovery, autonomy, and the ability of individuals to lead fulfilling lives outside of institutional settings. The goal should be to support people in achieving their highest level of independence and quality of life, not to confine them to institutional environments.
Third, proponents of re-opening səmiq̓ʷəʔelə/Riverview Hospital often argue that it would be a cost-effective strategy. This claim ignores the substantial costs associated with running a large-scale institution, including staffing, maintenance, and the associated bureaucratic overhead. Community-based care, while requiring investment, often proves more cost-effective in the long run by reducing emergency room visits, hospitalizations, and legal system interactions. Moreover, it fosters a more inclusive and supportive society. But again, funding and resources are needed along with a plan for affordable housing are required to support such a plan.
Finally, suggesting that we return to the institutional models of the past fails to recognize the profound changes in society and mental health care over the decades. Our understanding of mental health has advanced significantly, and the societal approach has shifted toward treatment that emphasizes integration and community support rather than isolation. Reverting to outdated methods would not only disregard these advancements but also ignore the lessons learned from past failures.
The calls to re-open səmiq̓ʷəʔelə/Riverview Hospital, spurred by recent violent incidents, reflect a misunderstanding of current mental health care practices and the progress we have made. It is imperative that we continue to invest in and refine our community-based mental health services, rather than looking back to a model that has long since been deemed ineffective and inadequate. Let us move forward with compassion and innovation, embracing the principles of modern mental health care.
-Michelle C. Danda, New Westminster