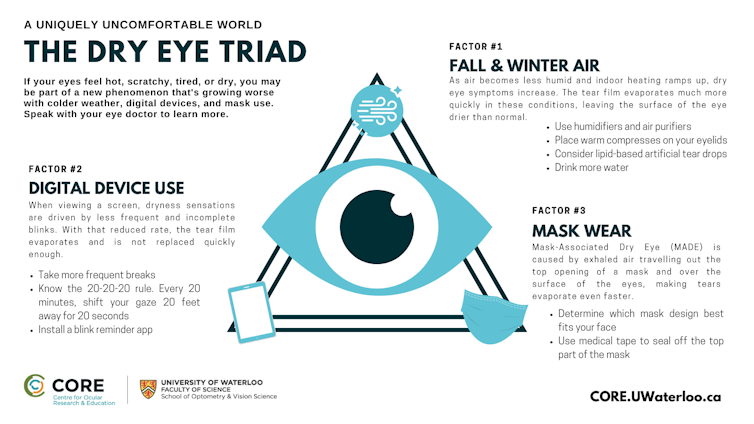
How do your eyes feel right now? Whether you’re sitting at home or in the office, you’re likely reading this on a digital device, and your eyes may be hot, scratchy, tired and dry. If so, you may be part of a new phenomenon called dry eye triad (DET).
The science of eye dryness has advanced rapidly in recent years, as has general awareness of the condition. Researchers have faced two new variables as the pandemic set in: significant upticks in digital screen use and altered airflow from mask wearing. Colder weather is on the horizon in much of the world, adding a seasonal third punch to a growing problem.
The good news is that people do not need to suffer in silence. Once aware of the causes and steps to counter dryness, everyday comfort is usually within reach.
What is dry eye disease?
Eye doctors report seeing more patients with irritated, burning and stinging eyes. These symptoms are very common, and when persistent can be diagnosed as dry eye disease, a condition affecting up to 75 per cent of the population.
Severity varies, with most people having minor intermittent symptoms, but for others it can be highly disruptive to work and daily life.
Dry eye disease has many causes, and effectively addressing it requires attention to multiple aspects of ocular health, general health and the environment.
Starting with the eye itself, the role of an eye care practitioner like me has been to ensure the eyelids and eyelashes are healthy, that the glands in the eyelids are producing oils, that there are sufficient tears to keep eyes feeling moist and ensure that surface inflammation is controlled. It is also important to account for health conditions and medications that may contribute to drying the ocular surface.
Then the pandemic arrived, behaviours changed and dry eye triad began to affect millions across the globe.
Factor 1: Impact of fall and winter
Your eyes are subject to the same environmental conditions as the rest of your body. This is more apparent during the fall and winter. As surrounding air becomes less humid, dry eye symptoms increase. Comfortable levels of humidity typically range between 40 and 70 per cent. During the coldest days of winter, humidity percentages can drop into the single digits. The tear film evaporates much more quickly in these conditions, leaving the surface of the eye drier than normal.
Cooler weather comes hand-in-hand with increased use of indoor heating. That commonly dry heat accelerates tear film evaporation even further.
Several steps can help offset these drying situations. Using humidifiers increases moisture in the air and air purifiers may also help.
Simple management strategies guard against excessive tear film evaporation by improving the oily (lipid) outer layer of the tear film. Using warm compresses on the eyelids helps tear film oils spread more easily, and adding lipid-based artificial tear drops supplements the oil level.
It also helps to drink more water to maintain adequate levels of hydration.
Factor 2: Increased digital device use
The COVID-19 pandemic has forced many people to work and study remotely from home, spending more time on digital devices. When viewing a screen, dryness sensations are driven by a change in blinking patterns. Blinks are less frequent and not as full and complete.
The natural mechanism of blinking is important to distribute a fresh layer of tears over the surface of the eye. With a reduced blink rate, the tear film evaporates and is not replaced quickly enough, leading to increased irritation and discomfort.
The most straightforward advice is to take more frequent breaks. The “20-20-20 rule” (every 20 minutes, look at something 20 feet away for 20 seconds) helps manage eye strain when working on digital devices. There are even programs and apps that remind you to blink more frequently and more fully.
Factor 3: Mask wear continues
With indoor mask-wearing still being mandated or recommended to reduce the spread of COVID-19, it has also resulted in some people noticing an increase in dry eye sensations. Termed mask-associated dry eye (MADE), it is caused by exhaled air travelling out the top opening of the mask and over the surface of the eyes, making tears evaporate even faster.
The remedy is similar to preventing glasses from fogging with mask wear: use medical tape to “seal off” the top part of the mask to prevent airflow there.
Managing dry eye triad
With winter drawing closer, plus increased digital device use and mask wearing, the dry eye triad’s triple-layered threat to the stability of your tear film is real. Thankfully, in most cases, that does not have to be debilitating.
Begin by having a conversation with your eye care provider, who can help you implement the steps I’ve mentioned to make sure your eyes are lubricated, well-rested and not subjected to low humidity and evaporative airflow conditions.
More intense eye dryness may well benefit from tailored treatment. Your optometrist or ophthalmologist may recommend a specific regimen or refer you to a dry eye speciality clinic. Several new pharmaceuticals and medical devices are putting relief in reach for even severe cases.
The most important advice of all, though, is not to dismiss dry eye altogether. The condition is real, more prevalent than ever and can be addressed with a combination of education, behaviours and therapies. Understanding your options will put you on a path to comfortable, healthy eyes not only during the cold weather months, but year-round.
William Ngo is a consultant with Alcon and Sun Pharma. William Ngo is an independent contractor (optometrist) at Market Lane Optical. William Ngo is a volunteer for the American Academy of Optometry. William Ngo has received awards and research funding from the American Academy of Optometry Foundation. As an employee at the Centre for Ocular Research & Education (CORE), we have received research funding from the following companies: Alcon, Allergan, Allied Innovations, Aurinia Pharma, Azura Ophthalmics, Bausch Health Canada, Brien Holden Vision Institute, CooperVision, GL Chemtec, i-MED Pharma, Johnson & Johnson Vision, Lubris, Menicon, Nature’s Way, Novartis, Ophtecs, Ote Pharma, PS Therapy, Santen, SightGlass, SightSage, Visioneering Tech Inc. CORE has also received funding from the following funding agencies: American Academy of Optometry Foundation, Natural Sciences and Engineering Research Council of Canada, Canadian Institutes of Health Research, Mitacs, Canadian Association of Optometrists, European Union Funding for Research & Innovation, Canada Foundation for Innovation, Innovation and Technology Commission.